California’s recently enacted $308 billion state budget included a $100.7 million program for the state to produce low-cost insulin. Of this amount, $50 million is earmarked for product development and $50 million is dedicated to building an in-state manufacturing facility.
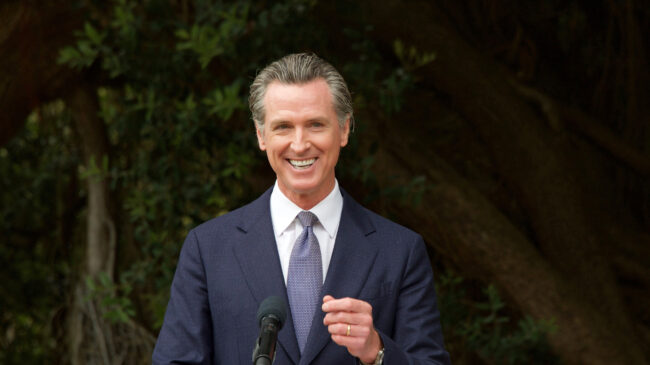
“Nothing epitomizes market failures more than the cost of insulin. Many Americans experience out-of-pocket costs anywhere from $300 to $500 per month for this life-saving drug,” Gov. Gavin Newsom remarked when announcing the passage of the insulin plan. “California is now taking matters into our own hands.”
While it is very unfortunate that Americans pay high prices for lifesaving insulin, high insulin prices are caused by a maze of regulation, bureaucracy, and pharmacy benefit managers that drive up the costs. While California’s efforts are well-intentioned, high insulin prices would be better addressed by regulatory reform and private initiative rather than a government-run program administered by a state with a dubious track record of competence and efficiency.
Evidence that the private sector can produce affordable insulin is available just south of the border. In Mexico, insulin prices are about one-sixth of those in the United States for a variety of reasons. Some Americans cross the border to take advantage of the lower costs. While it is illegal to import prescription drugs to the United States, the federal government generally does not enforce the prohibition for personal importation of up to a three-month supply of most medicines. But making regular trips to Mexico isn’t a sustainable solution for most California insulin users.
One problem in the United States is a lack of competition arising from patent protection for insulin delivery devices and barriers to getting approval for biosimilar products. There is some promise on the latter front as the Food and Drug Administration approved two biosimilars in 2021.
But additional reforms will likely be needed to bring US insulin prices down to international levels. Writing in Mayo Clinic Proceedings in 2020, the Mayo Clinic’s Dr. Vincent Rajkumar recommended that the United States participate in a reciprocal approval process with Canada and Western European countries. If a drug regulator in one of those nations approves a new insulin treatment, it could also be sold in the United States.
Further, Rajkumar recommended limiting the length of initial patents and preventing the use of additional patents on a single drug to extend market exclusivity. Although generous patent protection is defended as a means of encouraging innovation, incremental changes in how insulin is produced or delivered may not merit long exclusivity periods.
Costs could also be reduced if patients could obtain newer insulin formulations without a prescription. Early insulin formulations are still available on a non-prescription basis, having been grandfathered in before the Food and Drug Administration acquired the authority to classify new drugs as prescription-only. Although non-prescription insulin accounts for a small portion of the market, its availability without publicized safety incidents likely suggests that all insulin formulations could be safely dispensed without a prescription.
Some price relief might also come from disruptive new market entrants such as Civica RX, a nonprofit generic drug company that plans to sell insulin for $30 per vial. Civica was founded in 2018 with the support of major health systems, including the Mayo Clinic, and large philanthropies (one of which also supports my employer, Reason Foundation). Nonprofits that prioritize delivering social benefits over net income can reasonably be considered a market response since they address consumer needs without the coercion and top-down thinking that characterizes government interventions.
For-profit companies can also address the high price of insulin. Mark Cuban’s Cost Plus Drug Company is offering prescription drugs at steep discounts by selling direct to consumers, eliminating markups imposed by pharmacy benefit managers and other middlemen. Cuban’s company appears to be working on adding insulin to its low-cost generic drug offerings.
Meanwhile, the same state government considering entering the complex pharmaceutical industry is struggling with basics, like upgrading its own computers and information technology systems. Rather than take a state-driven insulin approach, California could more effectively bring down insulin prices by importing it or purchasing it from new entrants like Civica RX and Cuban’s company.